Emotional wellbeing outcomes: prevalence and reasons why
Click on any of the headings below to find out more information.
- 82% of midwives in this sample reported feeling unwell due to work-related stress in the past year.
- There was no significant difference in the levels of work-related stress between regions of the UK when all relevant factors were considered.
- Less than a third of midwives took time off work because of work-related stress.
- The most common reasons for not taking time off work were because of the impact this may have on colleagues or service.
What were the reasons midwives felt contributed to work-related stress?
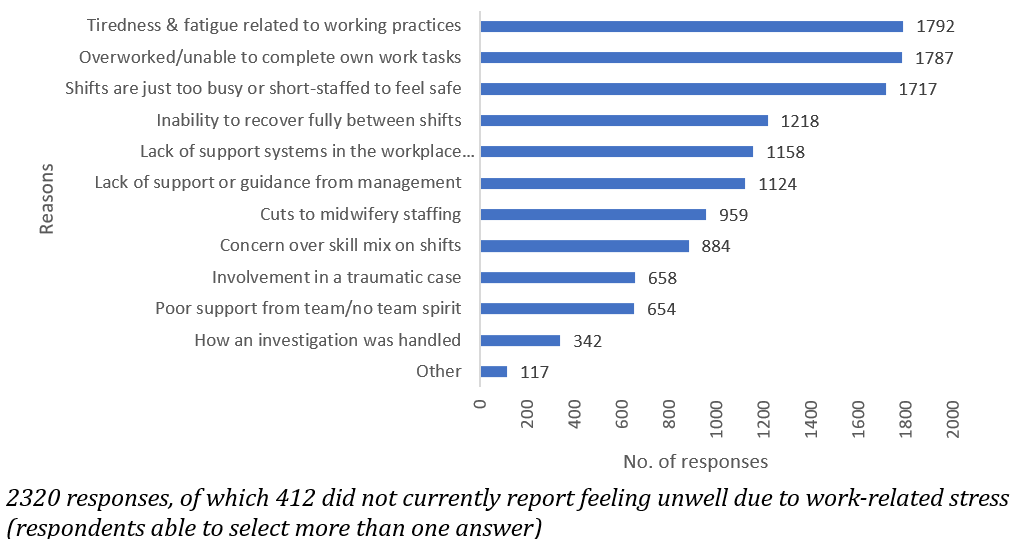
Other factors: blame culture or bullying; changes in service provision, including the implementation of the continuity of care models; attitudes and behaviours of managers; administrative or IT issues; redeployment.
In this study, burnout was calculated as a score of 50 or more on the Copenhagen Burnout Inventory. This does not mean that burnout was not present in those with scores less than 50, but this cut-off point was used for analytical purposes.
- 77% of midwives in this sample had personal burnout.
- 83% of midwives in this sample had work-related burnout.
- 17% of midwives in this sample had client-related burnout.
There was no significant difference in the levels of burnout between regions of the UK when all relevant factors were considered.
- Just less than 40% of midwives in this sample were satisfied with their level of job satisfaction (3% of these strongly agreed).
- There was no significant difference in the levels of job satisfaction between regions of the UK when all relevant factors were considered.
Factors Contributing to Job Satisfaction:
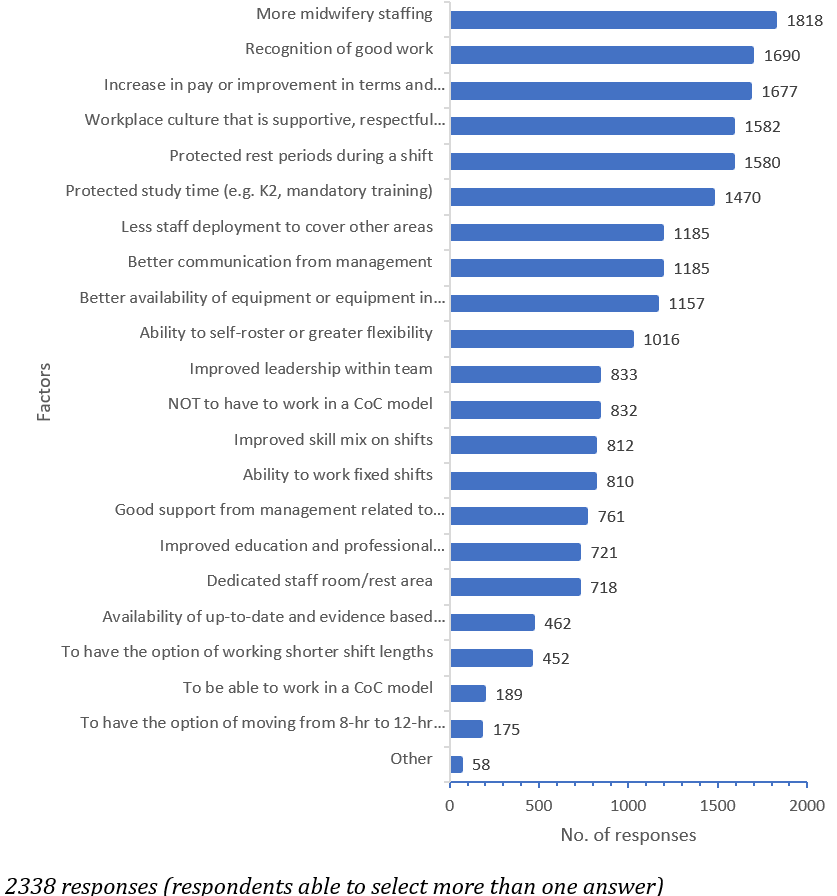
Other factors included improvements in admin or functionality of IT systems, consideration of personal lives/flexible working, smaller caseloads and adequate training support.
The extent that midwives were pleased with the standard of care they could provide was used as an additional indicator of job satisfaction:
- 50.5% of midwives in this sample agreed that they were able to do their job to a standard they were pleased with (6% of these strongly agreed).
- There were significant differences between regions (see menu 'Other factors')
What were the factors midwives felt most negatively impacted on the standard of care they could provide?
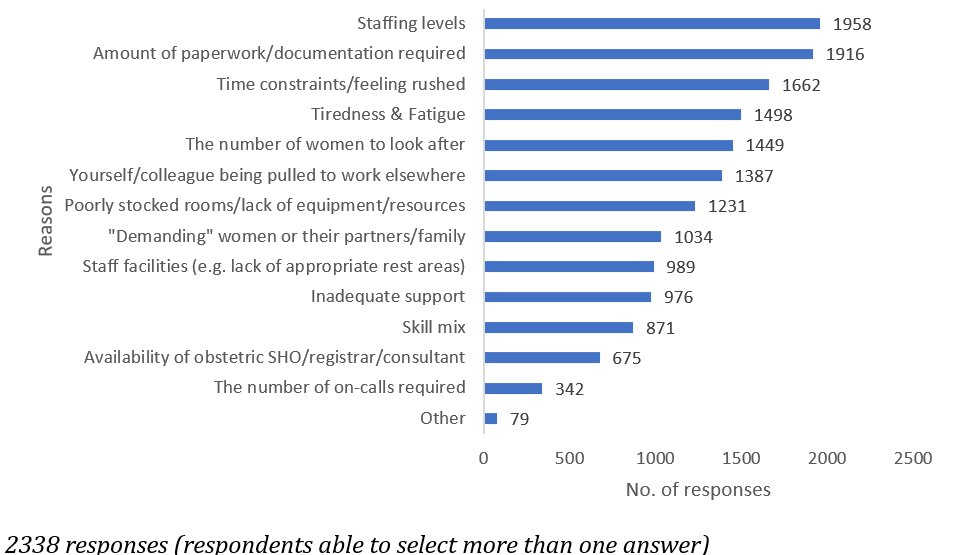
Other factors included lack of management, unreasonable expectations, management working to different goals, such as box ticking and poor communication.
Ever having thoughts about leaving midwifery was used as an additional indicator of job satisfaction:
- 76% of midwives in this sample had thought about leaving midwifery.
- There was no significant difference in the levels of thinking about leaving between regions of the UK when all relevant factors were considered.
What were the reasons that midwives gave for thinking about leaving midwifery?
Over 25% thought about leaving because the continuity of care model does not fit their lifestyle, but this differed by region. Over 40% in the North East of England felt this was a factor, but it was less than 2% in Wales.
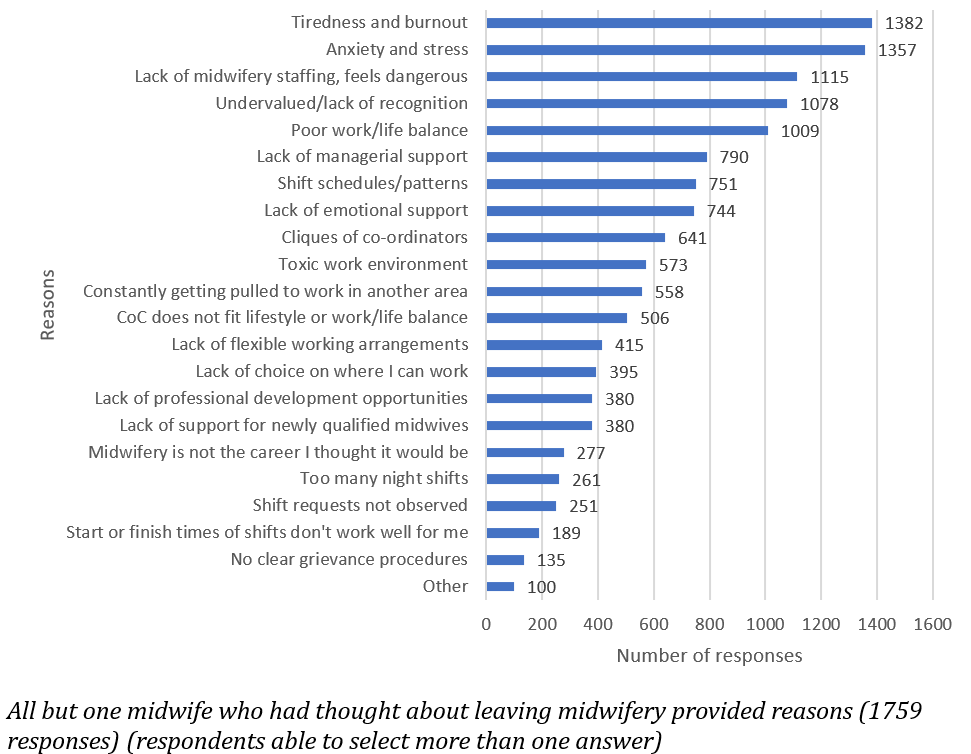
There was wide variation in other reasons given, including too many on-calls so unable to recover; bullying and attitude within work environment; pay; litigation; blame culture or defensive practice.