What did the working practices of NHS midwives look like?
Click on any of the headings below to find out more information.
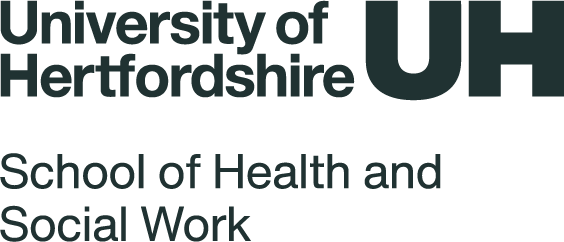
- 12-hour shifts were the most common shift length worked, particularly for night shifts.
- Eight-hour shifts were still routinely in operation, most commonly in community or integrated care settings (62%).
- Scotland had the highest proportion of midwives scheduled to work 8-hour day shifts (45%).
- Shifts in excess of 12.5 hours were more common in the South West of England and in the North East (18% both regions).
- Over half of all midwives were required to work mixed shift lengths, either to make up weekly hours or because of study days, training or other reasons.
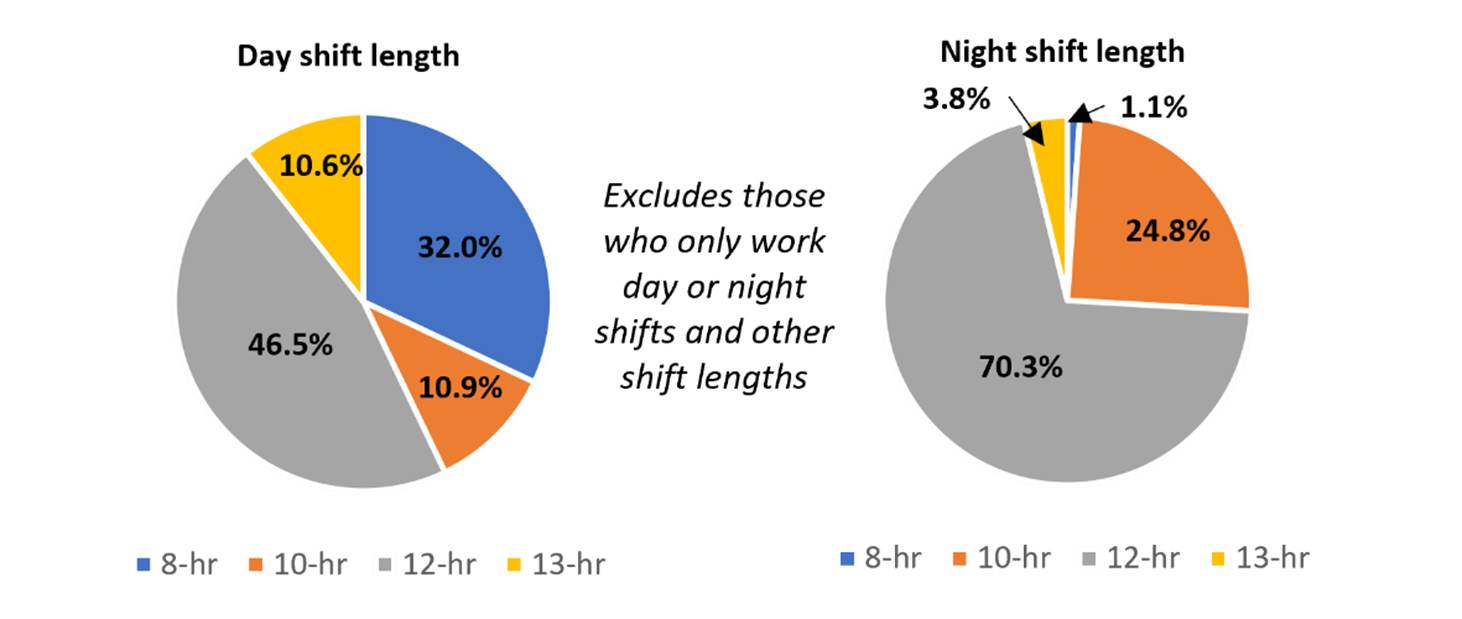
- In this sample, 36% of midwives were required to work on-calls.
- On-call working was more common in community, continuity of care teams or in integrated units (mix of community and hospital) (62%), with the remainder based in hospital settings.
- The number of on-calls in a 4-week period ranged from less than one to 20, with the most common being 1 to 2 a month (39%), followed by 3 to 4 a month (30%).
- The average number of on-calls worked was significantly greater for those working in continuity of care models compared to those working in community (all regions except Northern Ireland as no midwives worked in a continuity of care model).
- Most midwives who were required to work on-calls had no formal methods in place to ensure their working pattern and on-calls allowed them sufficient recovery time before being back on duty.
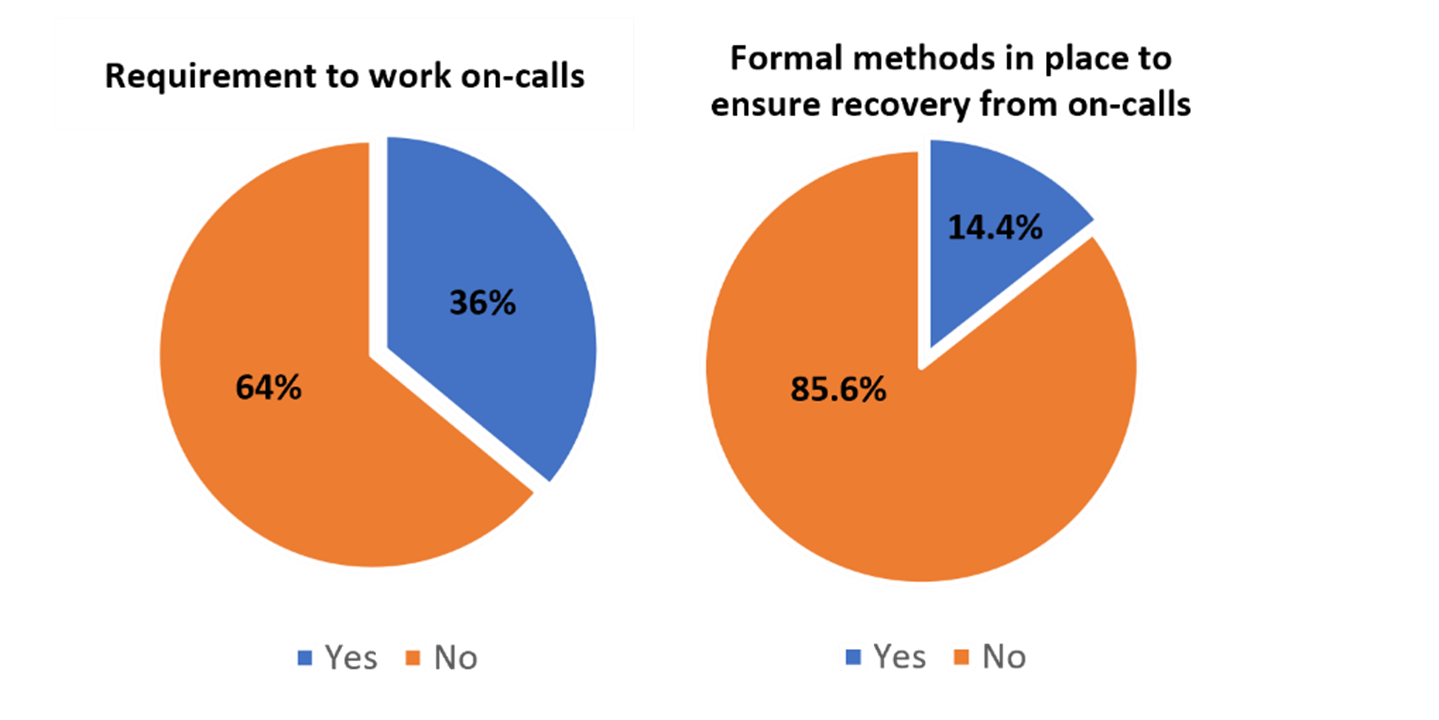
- Most midwives received their off-duty (detailing the shifts they are scheduled to work) at least four weeks in advance of their scheduled shifts.
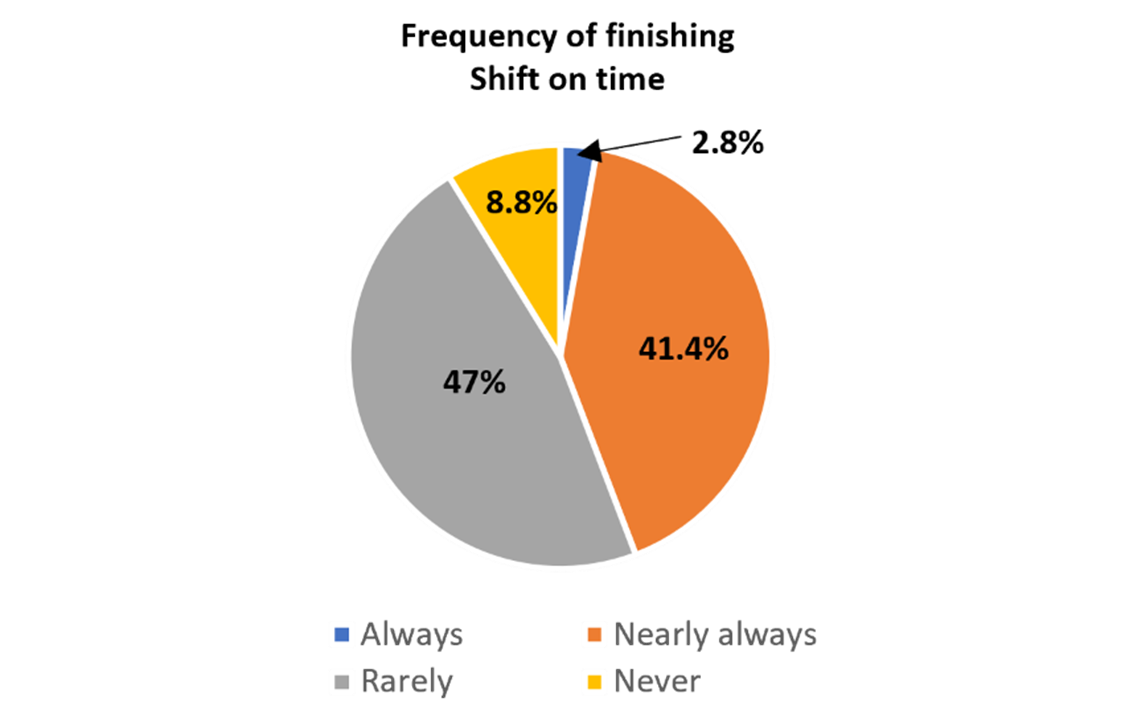
- More than half of all midwives had rarely or never finished their shift on time in the previous month.
What were the reasons midwives gave for not finishing their shift on time?
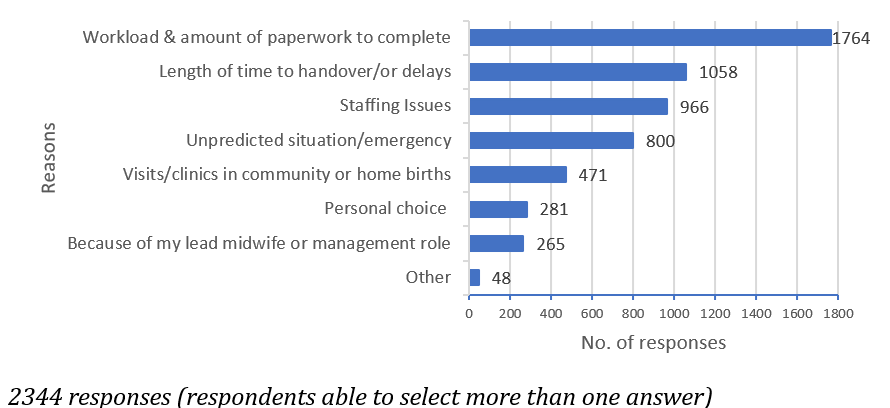
Other reasons include administrative or IT issues, clinics overrunning, community midwives' travel time not included in diary bookings, dealing with student issues, redeployment, completion of mandatory training, safeguarding issues, support/debrief for fellow midwives, and the flexible nature required to provide women with continuity.
- Around half of midwives had a one-hour break, whether taken as one break or split into two 30-minute breaks.
- 42% of midwives had a 30-minute break (more common in 8-hour shifts, but also seen for shifts of 10-11.5 or 12.5 hours)
- 20% of midwives working 10-11.5 hour shifts had a 20-minute break
- 12.5% of midwives working 12.5-hour shifts had a 20-minute break
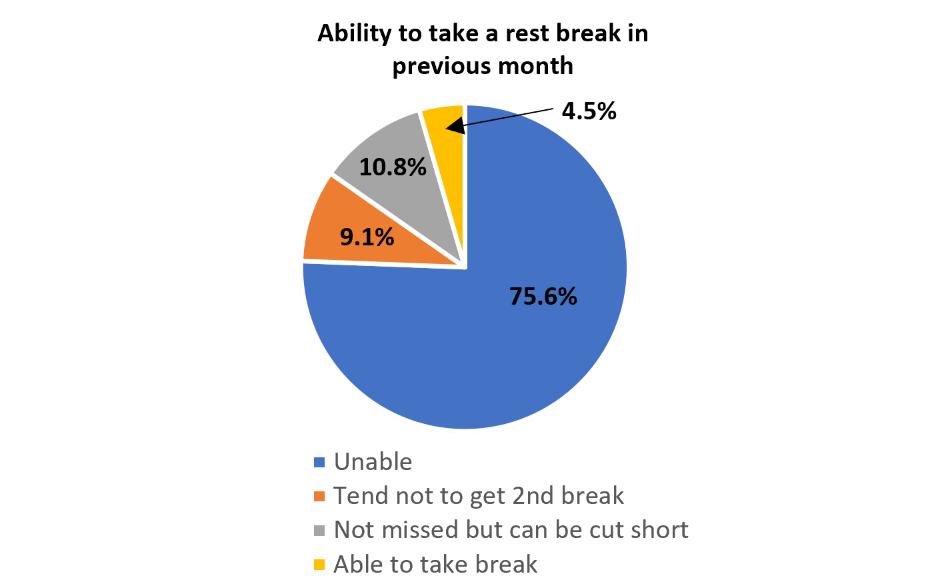
- Less than 5% of the midwives in this sample had been able to take all their allocated breaks in the previous month. ‘Tend not to get 2nd break’ relates to when a break is split into two.
What were the reasons midwives gave for not being able to take a rest break or for it being cut short?
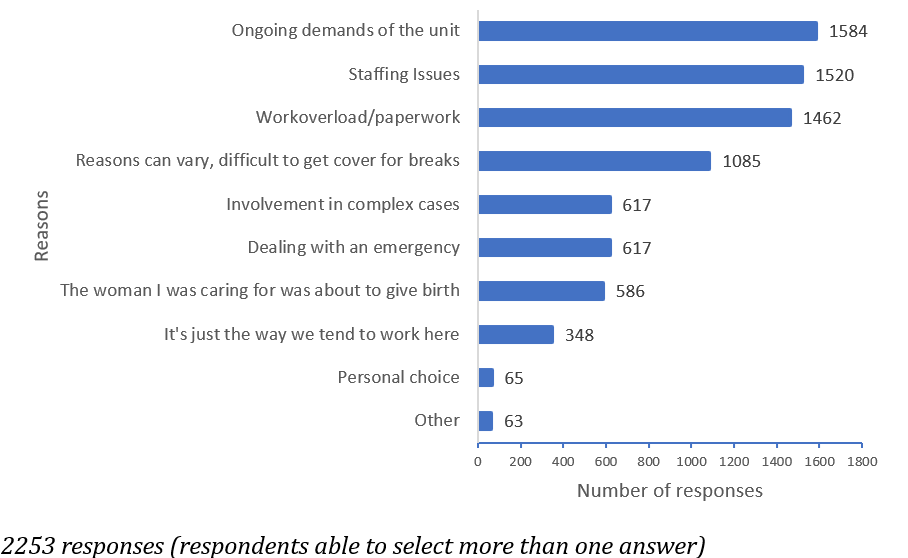
Other:Related to work environment, culture of logistics (such as lack of rest areas or facilities, poor timing of breaks, administrative or IT issues).
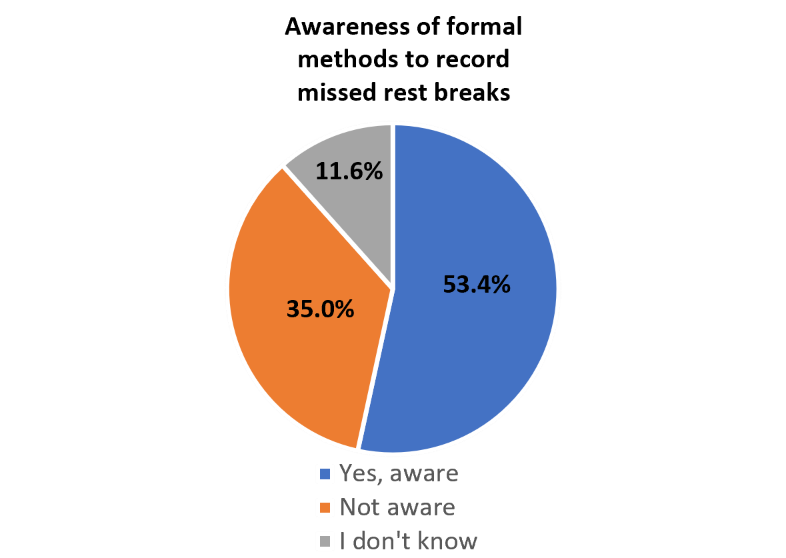
Just over half of midwives reported that there was a formal method in place to record missed rest breaks.
- In this sample, 22% of midwives only worked day shifts, and just under 2% only worked night shifts.
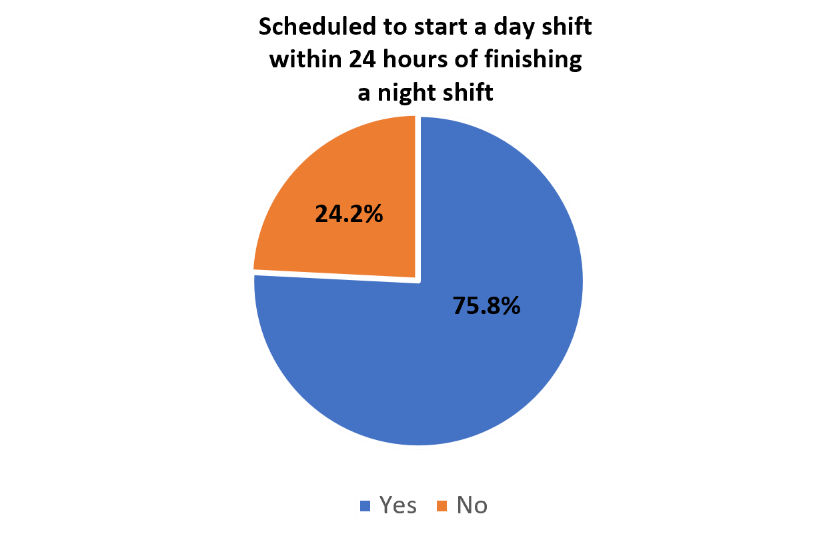
- Of the remaining midwives, over three-quarters were scheduled to start a day shift within 24 hours of finishing a night shift (for example, finishing a Sunday night shift at 8.15 on Monday morning, but having to be back at work to start a day shift at 7.45am on the Tuesday).
- Half of midwives reported being called away from a mandatory training session in the past year to provide clinical care in the unit.
- Over three-quarters of midwives said this was due to ‘generally inadequate staffing’. Other reasons included unexpected high activity levels or to cover staff sickness.